Catherine Burns
Health correspondent
Vicki Loader
Health producer
 BBC
BBC
More than 1,000 GPs in England have shared their views about the assisted dying bill with BBC News
If you ask these three doctors about being GPs, their answers are remarkably similar.
"It can be the best job in the world," one tells me. It's "a privilege" another says. They all talk about how they love getting to know their patients and their families.
But all three have different views on assisted dying.
Right now, the law here is clear: medics cannot help patients to take their own lives. But that could change.
The Terminally Ill Adults (End of Life) Bill is being debated in Parliament. And if it goes through, it will give some terminally ill patients in England and Wales the option of an assisted death.
Here, three doctors - Abdul Farooq, Susi Caesar and Gurpreet Khaira, who all have a different view on assisted dying - tell us how they feel about the proposals.
'A red line I would never cross'
Dr Abdul Farooq is 28 and relatively new to his career as a GP.
We meet at his home in east London. He gives his baby daughter a bottle of milk before heading around the corner to pray in his local mosque.
His religion is absolutely key to his views on assisted dying.
"I believe in the sanctity of life. As a Muslim, I believe that life is a gift from God, and that no one has the right to take that away," he says.
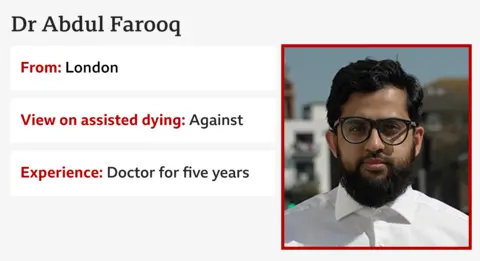
Dr Farooq feels taking your own life is wrong, and so, he says, it would be "sinful" for him to be involved in that process - even indirectly.
If this law passed - and a patient came to him asking for help to die - he would refer them to another doctor.
He says anything beyond that would be "a red line I would never cross".
Dr Farooq's objections are also informed by his professional experience, particularly his time working in a hospital.
He describes seeing "undignified deaths" - people passing away on busy wards - and says the health system is not getting the basics right in end-of-life care.
"There is so much we can do to make patients comfortable, if we have the right resources available," he tells me.
"We have a whole field of medicine called palliative medicine that is there to help people towards the end of their life. So why are we not throwing all our resources and money into that and actually making the process of death less scary?"
He's also concerned about specific parts of the proposed law. Doctors would have to assess if terminally ill patients are expected to die within six months before they are approved for an assisted death.
Dr Farooq sees this as problematic. The final day or so is easy to predict, he says, but adds that some patients he's expected to die within six months can still be alive a year later.
Is there anything that could change his mind on assisted dying?
"No," Dr Farooq says without hesitation. "I'm strongly against it. Personally and professionally, I think it's the wrong thing to do for patients."
'I'll be at the front of the queue to help'
Dr Susi Caesar has been a GP for 30 years and thinks she probably wouldn't have previously been so vocal in her support of assisted dying.
Now, she says she is ready to "stick her head above the parapet".
Recently she lost her beloved dad, Henning. We meet at a lake near Cirencester because being near water reminds her of him.
"My father was the most amazing person and this is so evocative of everything he loved," she says. "The outdoors, walks, sailing, boats, kayaking, swimming."

She thinks Henning would be proud of her for talking to us about her views because he was a long-term believer in assisted dying.
When he was diagnosed with a terminal illness, Dr Caesar says he became "terribly scared about the manner of his dying".
"My father was a very proud man, and the thing that was unbearable to him was the idea that he would lose control at the end of his life - of his bodily functions, of his mind, of his ability to be the person that he was."
By the end, Dr Caesar says her father's "medication never quite kept up with his symptoms." For her, the argument over assisted dying comes down to patient choice.
"Everybody is going to die. Every individual deserves the comfort of choice about how they die. I would want it for myself," she tells me.
She acknowledges that many of her colleagues have "very, very reasonable concerns" about assisted dying. But she says "we have the wisdom to set up systems that will work and get over some of these hurdles."
I ask if Dr Caesar's support for assisted dying would translate into her working in this area.
"I will be at the front of the queue to help people to have the death that they wanted," she says. "I think that's the core joy of my job - being with people to the very end of their health journey."
'A very guilty place'
Dr Gurpreet Khaira doesn't have any of the certainty of Dr Farooq and Dr Caesar.
She describes herself as "pretty conflicted about the whole subject" of assisted dying.
Dr Khaira is a GP in Birmingham but also has first-hand experience as a patient.
In 2017, she was diagnosed with breast cancer. She found chemotherapy gruelling and says if the cancer ever came back, she wouldn't want to go through it again.

"I remember feeling very passionate that I should have the choice of whether I go through this kind of treatment, or to say 'that's enough now'," she says.
She says it felt very important for her to have a choice about the end of her life.
Now, she's a picture of health, striding along a hillside with ease.
As a GP with decades of experience, she worries that vulnerable patients might opt for assisted dying rather than be a burden to their loved ones. Or that some families might coerce vulnerable patients into it.
"That is one of my biggest areas of personal conflict. I know that there are lots of plans to put safeguards in.
"You can be the best doctor or advocate in the world, but you may not pick up where someone is being controlled or manipulated."
For her, there's a fundamental conflict between her personal and professional experiences.
But, she adds: "As a doctor, I'd be very reluctant to be handing over a syringe for a patient to make that choice."
Balancing up these two sides leaves her "in a very guilty place", she says, but adds that it's not a weakness to be open minded. For her, making this decision is an "evolving process".
Personal experience shaping opinions
It's striking when talking to Dr Farooq, Dr Caesar and Dr Khaira, how much their views on assisted dying reflect their core belief systems.
In that respect, GPs are possibly much like the rest of us.
If this bill does pass into law, doctors will have to consider whether they are willing to work in the area of assisted dying, or not. They could be asked to be involved in the process - whether that's holding preliminary discussions with patients who want to die, to prescribing a substance for someone to end their own life.
If they don't want to, no-one will force them.
They will have time to think about it. If MPs do vote in favour of this next month, it could still take years to come into effect.
.png)
 German (DE)
German (DE)  English (US)
English (US)  Spanish (ES)
Spanish (ES)  French (FR)
French (FR)  Hindi (IN)
Hindi (IN)  Italian (IT)
Italian (IT)  Russian (RU)
Russian (RU) 








Comments