
NEW DELHI: In a rare surgical procedure, doctors at AIIMS successfully conducted a procedure to separate a ‘parasitic twin’ weighing 15 kg from a 17-year-old boy hailing from UP’s Unnao district. The occurrence of conjoined twins is notably uncommon, with frequencies of 1 in 50,000 to 100,000 births. In certain instances, incomplete development results in asymmetrical or ‘parasitic twins’, where one twin (autosite) develops fully while the other (parasite) remains dependent. Such cases are exceedingly rare, with only 40 documented instances in world medical literature.
Dr Asuri Krishna, additional professor in the surgery department, noted that when the boy visited AIIMS OPD on Jan 28, they initially mistook his covered abdomen for a carried child. Instead, they discovered two fully developed lower limbs with external genitalia attached to his abdomen.
Freed from ‘parasitic twin’, boy makes quick recovery
Since birth, the boy lived with these additional limbs from his underdeveloped twin. The parasitic appendage, including underdeveloped male genitalia, grew proportionally with him. The boy experienced sensations, including touch, pain and temperature in the parasitic limb. Despite occasional abdominal discomfort, he maintained normal bodily functions without major health complications.
His condition led to considerable social isolation and emotional difficulties throughout childhood. Local medical practitioners advised against removal, warning of potential fatality due to shared cardiac connections. These circumstances forced him to discontinue his education after 8 years of age. His physical limitations included the inability to sleep on his abdomen.
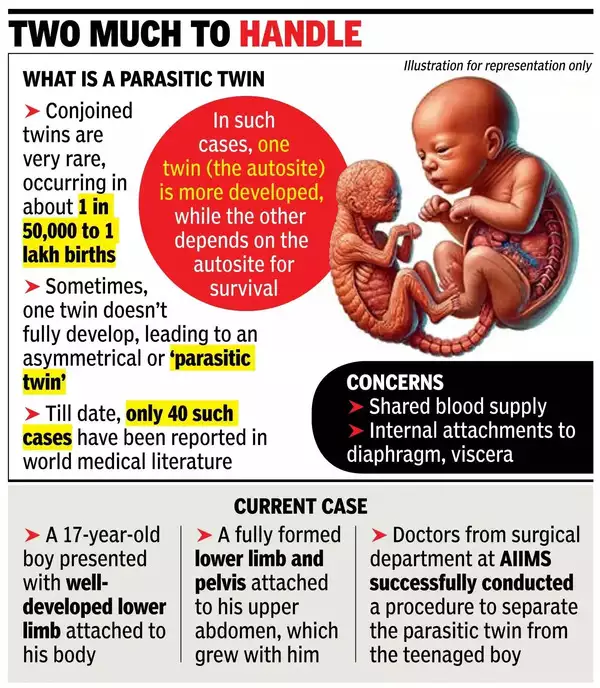
The parasitic structure received nutrition through blood supply from the host twin. Medical experts noted that as patients age, such parasitic growths can potentially cause cardiovascular complications and neurological issues, posing life-threatening risks.
Following a relative's suggestion, he sought treatment at AIIMS as a last hope. Upon arrival, a multidisciplinary team, including surgeons, radiologists and anaesthesiologists evaluated his condition.
AIIMS specialists noted that whilst prenatal screening can detect this condition, the patient's socio-economic background prevented early diagnosis.
CT angiography revealed the parasitic limb's blood supply originated from an internal mammary artery branch. The scan also identified a substantial abdominal cystic mass. After comprehensive preparation, surgery was scheduled for February 8, 2025.
The complex procedure involved two phases: removing the parasitic limb through careful dissection and vessel ligation, followed by excision of the abdominal cystic mass.
Surgeons discovered and removed underdeveloped testes within the attachment site tissue. The second phase required careful separation of the cystic mass from surrounding organs. They noted an unusually high bladder extension, which required precise surgical management. Post-procedure drainage and suturing completed the operation. The operation lasted between 2 and 2.5 hours.
Doctors said that the patient was free from additional health complications. Recovery was swift, with successful oral feeding resuming the next day. The medical team removed the drain on the third day, and the patient was cleared to go home on the fourth day.
After 17 years of physical and emotional challenges, the successful surgery brought immense relief. Initially experiencing phantom sensations, the patient could finally anticipate a conventional lifestyle.
The achievement resulted from collaborative efforts of numerous specialists, including Dr Asuri Krishna, Dr VK Bansal, Dr Sushant Soren, Dr Brijesh Kumar Singh, Dr Abhinav Kumar, Dr Jaymeen Makwana from Surgical Disciplines, Dr Manish Singhal and Dr Sashank from plastic surgery, Dr Ganga Prasad and Dr Rakesh from anaesthesia, and Dr Atin and Dr Ankita from radiology.
.png)
 German (DE)
German (DE)  English (US)
English (US)  Spanish (ES)
Spanish (ES)  French (FR)
French (FR)  Hindi (IN)
Hindi (IN)  Italian (IT)
Italian (IT)  Russian (RU)
Russian (RU)  6 hours ago
2
6 hours ago
2








Comments